Piriformis Syndrome Surgery
- Miami -
overview
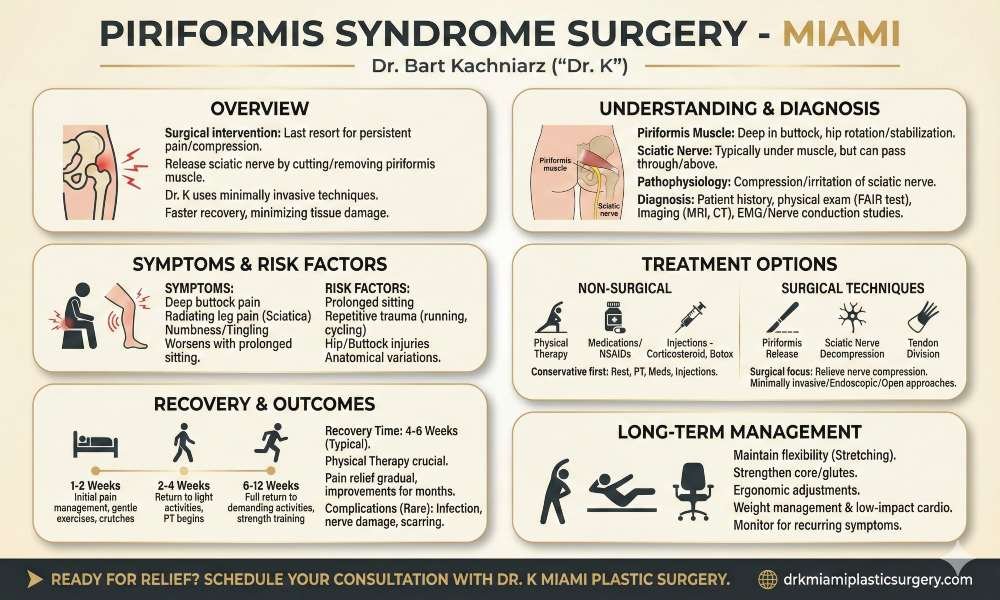
Piriformis syndrome can cause persistent pain and discomfort in the buttocks, hips, and legs, significantly impacting daily activities and quality of life. When conservative treatments fail to provide relief, surgery may be considered as a last resort. Surgical intervention for piriformis syndrome aims to release the compressed sciatic nerve by cutting or partially removing the piriformis muscle.
The decision to undergo surgery requires careful consideration and evaluation by a qualified specialist. Dr Kachniarz employs employ minimally invasive techniques to access and release the piriformis muscle, minimizing tissue damage and promoting faster recovery. While success rates vary, many patients experience significant improvement in symptoms following the procedure.
Get in touch with us at Dr K Miami and see if we can help.


Understanding Piriformis Syndrome
The piriformis muscle is a small, pear-shaped muscle located deep in the buttock. It originates from the sacrum and attaches to the greater trochanter of the femur. The muscle plays a crucial role in hip rotation and stabilization.
The sciatic nerve typically passes beneath the piriformis muscle. However, in some individuals, the nerve may pass through or above the muscle, increasing the risk of compression.
The piriformis muscle works in conjunction with other external rotators of the hip, including the gluteus maximus. Its primary function is to externally rotate the hip when the leg is extended and abduct the hip when the leg is flexed.
Pathophysiology
Piriformis syndrome occurs when the piriformis muscle compresses or irritates the sciatic nerve. This compression can result from muscle hypertrophy, inflammation, or anatomical variations.
Factors contributing to piriformis syndrome include:
- Muscle spasm or tightness
- Trauma or injury to the buttock area
- Anatomical anomalies of the muscle or nerve
- Prolonged sitting or repetitive activities
Compression of the sciatic nerve can lead to inflammation, causing pain, numbness, and tingling along the nerve’s path. In some cases, the syndrome may develop due to changes in muscle tension or movement patterns.
Epidemiology and Risk Factors
Piriformis syndrome is relatively uncommon, affecting approximately 6-8% of individuals with lower back pain. It is more prevalent in women, possibly due to differences in pelvic anatomy.
Risk factors include:
- Prolonged sitting or standing
- Repetitive trauma from activities like running or cycling
- Previous hip or buttock injuries
- Anatomical variations in muscle or nerve positioning
- Leg length discrepancy
Occupations requiring prolonged sitting or repetitive hip movements may increase the risk of developing piriformis syndrome. Athletes participating in activities involving frequent hip rotation are also at higher risk.
Signs and Symptoms
The primary symptoms of piriformis syndrome include:
- Buttock pain, often described as deep and aching
- Sciatica-like pain radiating down the leg
- Numbness or tingling in the buttock and leg
- Pain worsening with prolonged sitting or activity
Additional signs may include:
- Tenderness in the buttock area
- Pain during hip rotation or stretching
- Difficulty sitting or walking for extended periods
- Reduced range of motion in the hip
Symptoms typically worsen with activities that engage the piriformis muscle, such as climbing stairs or running. Pain may also increase when sitting on hard surfaces or crossing legs.
Differential Diagnosis
Accurately diagnosing piriformis syndrome can be challenging due to its similarity to other conditions. Healthcare providers must consider several potential causes of buttock and leg pain:
- Lumbar radiculopathy
- Spinal stenosis
- Herniated disc
- Deep gluteal syndrome
- Hamstring tendinopathy
- Sacroiliac joint dysfunction
Imaging studies, such as MRI or CT scans, may be necessary to rule out other conditions. Electromyography and nerve conduction studies can help assess nerve function and identify areas of compression.
A thorough physical examination, including specific tests like the FAIR (Flexion, Adduction, and Internal Rotation) test, can aid in diagnosis. Providers may also use diagnostic injections to confirm the involvement of the piriformis muscle.
Diagnosis of Piriformis Syndrome
The clinical evaluation begins with a thorough patient history and physical examination. Patients typically report buttock pain that may radiate down the leg. The pain often worsens with prolonged sitting or activities involving hip rotation. During the physical exam, the practitioner assesses for tenderness in the buttock area and performs specific tests to evaluate piriformis muscle tension.
One common test is the FAIR (Flexion, Adduction, and Internal Rotation) test. The patient lies on their back while the examiner flexes, adducts, and internally rotates the affected hip. A positive result occurs if this maneuver reproduces the patient’s symptoms.
Another useful test is the Freiberg’s sign. The examiner applies pressure to the piriformis muscle while the patient lies on their side. Pain indicates a positive result.
1. Imaging Techniques
While imaging is not always necessary, it can be valuable in ruling out other conditions and confirming the diagnosis. Magnetic Resonance Imaging (MRI) is the preferred imaging method for piriformis syndrome. It can reveal inflammation, swelling, or anatomical variations of the piriformis muscle and its relationship to the sciatic nerve.
Computed Tomography (CT) scans may be used to assess bony structures and detect any space-occupying lesions. Ultrasonography can provide real-time imaging of the piriformis muscle and surrounding structures, allowing for dynamic evaluation during movement.
Magnetic Resonance Neurography, a specialized MRI technique, can visualize the sciatic nerve and detect any compression or irritation.
2. Nerve Conduction Studies
Electromyography (EMG) and nerve conduction studies play a crucial role in diagnosing piriformis syndrome. These tests evaluate the function of nerves and muscles in the affected area.
EMG can detect abnormal electrical activity in the piriformis muscle and surrounding muscles. It may reveal signs of denervation or muscle irritability consistent with nerve compression.
Nerve conduction studies assess the speed and strength of electrical signals along the sciatic nerve. Slowed conduction or reduced signal amplitude in the affected leg can indicate nerve compression at the level of the piriformis muscle.
3. Diagnostic Criteria
No universally accepted diagnostic criteria exist for piriformis syndrome. However, several key factors are considered:
- Buttock pain with or without radiation down the leg
- Tenderness over the piriformis muscle
- Pain exacerbation with prolonged sitting or specific movements
- Positive results on provocative tests (e.g., FAIR test, Freiberg’s sign)
- Absence of lumbar spine pathology or other clear causes of symptoms
- Supportive findings on imaging or nerve conduction studies
A combination of these factors, along with a careful exclusion of other potential causes, guides the diagnosis of piriformis syndrome. The practitioner must consider the overall clinical picture and rule out conditions such as lumbar radiculopathy, hip pathology, or pelvic disorders before confirming the diagnosis.


Meet Your Doctor
With years of experience in the field of plastic surgery, Dr. K has built a reputation as one of Miami’s premier plastic surgeons.
His journey into medicine began with a passion for helping others and a keen eye for detail—qualities that have defined his career ever since, but what truly sets him apart is his genuine care for each patient who walks through our doors.
SEE WHAT WE CAN DO FOR YOU
Non-Surgical Treatment Options
- Conservative Management
Conservative management of piriformis syndrome typically begins with rest and activity modification. Patients are advised to avoid activities that exacerbate symptoms. Physical therapy plays a crucial role in treatment, incorporating stretching exercises to improve flexibility of the piriformis muscle and surrounding tissues. Strengthening exercises for the hip and core muscles help stabilize the pelvis and reduce pressure on the sciatic nerve.
Heat and cold therapy can provide relief from pain and muscle spasms. Massage techniques may be employed to relax tight muscles and improve circulation. Ultrasound therapy is sometimes used to reduce inflammation and promote healing.
- Medications and Injections
Various medications can help manage piriformis syndrome symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen are commonly prescribed to reduce pain and inflammation. For severe cases, muscle relaxants may be used to alleviate muscle spasms.
Localized injections are another treatment option. Corticosteroid injections can provide significant pain relief and reduce inflammation around the piriformis muscle. These injections are often guided by ultrasound or fluoroscopy for precise placement.
Botulinum toxin injections have shown promise in some cases, particularly for patients with muscle spasms. They work by temporarily paralyzing the piriformis muscle, potentially relieving compression on the sciatic nerve.

Surgical Treatment Options
Surgery becomes an option when non-surgical treatments prove ineffective after several months. Patients with persistent buttock and leg pain, muscle weakness, or numbness may be candidates. Imaging studies showing piriformis muscle anomalies or sciatic nerve compression can support the decision for surgical intervention.
Severe cases with significant nerve compression or muscle hypertrophy are more likely to require surgery. Chronic cases lasting over 6 months despite conservative management may also benefit from surgical approaches. The decision involves careful evaluation of symptoms, functional limitations, and quality of life impact.
Piriformis Syndrome Surgery Techniques
Surgical techniques for piriformis syndrome focus on relieving sciatic nerve compression. Common approaches include:
- Piriformis release: Involves cutting the piriformis muscle to reduce tension on the sciatic nerve.
- Sciatic nerve decompression: Removes scar tissue or adhesions around the nerve.
- Tendon division: Cuts the tendon attaching the piriformis to the femur.
Minimally invasive techniques use small incisions and specialized instruments to access the piriformis region. These methods aim to reduce tissue damage and promote faster recovery. Endoscopic approaches allow visualization of the sciatic nerve and piriformis muscle through small portals.
Open surgery may be necessary for complex cases or when extensive scar tissue is present. This technique provides direct access to the piriformis muscle and sciatic nerve but involves a larger incision.

Postoperative Management
Recovery after piriformis syndrome surgery typically involves a structured rehabilitation program. Initial focus is on pain management and wound care. Patients usually start gentle exercises within days of surgery to prevent stiffness.
Physical therapy plays a crucial role in recovery. Early interventions include:
- Range of motion exercises
- Gradual strengthening of hip and core muscles
- Gait training
Most patients can return to light activities within 2-4 weeks. Full recovery may take 6-12 weeks, depending on the surgical technique and individual factors. Follow-up appointments monitor progress and address any complications.
Pain relief is often gradual, with improvements continuing for several months post-surgery. Patients are advised to avoid prolonged sitting and heavy lifting during the initial recovery period.
Surgical Alternatives
While surgery is effective for many, alternative treatments may be considered:
- Botulinum toxin injections: Temporarily paralyze the piriformis muscle, reducing nerve compression.
- Radiofrequency ablation: Uses heat to disrupt nerve signals, potentially alleviating pain.
- Peripheral nerve stimulation: Implants a small device to deliver electrical pulses, modulating pain signals.
These alternatives may be suitable for patients who are poor surgical candidates or prefer less invasive options. Success rates vary, and multiple sessions may be required for optimal results.
Emerging techniques like ultrasound-guided procedures offer promising results with minimal invasiveness. However, long-term outcomes and comparisons to traditional surgery are still being studied.
Complications of Surgery
Infection is a risk with any surgical procedure. Patients may experience fever, redness, or drainage at the incision site. Nerve damage can occur, potentially causing numbness, weakness, or increased pain. Bleeding and hematoma formation are possible complications.
Scarring may develop around the surgical area, potentially leading to adhesions. In rare cases, this could cause recurrent symptoms. Some patients report temporary or prolonged muscle weakness in the affected leg.
Anesthesia-related complications, while uncommon, can include allergic reactions or respiratory issues. Blood clots, though rare, pose a risk, particularly in patients with limited mobility during recovery.
Recovery
Recovery time varies but typically ranges from 4 to 6 weeks. Initial days post-surgery focus on pain management and wound care. Patients often use crutches or a cane for the first week to reduce pressure on the affected area.
Physical therapy usually begins within 1-2 weeks after surgery. Early exercises focus on gentle stretching and range of motion. As healing progresses, strength training is incorporated.
Most patients can return to desk jobs within 2-3 weeks. Full return to physically demanding work or sports may take 6-12 weeks. Pain and discomfort generally decrease gradually over this period.
Swelling and bruising are common in the first weeks. Ice therapy and elevation help manage these symptoms. Patients typically see significant improvement in sciatic pain symptoms within the first month post-surgery.
Long-Term Management
Maintaining flexibility through regular stretching is crucial for long-term success. Focus on piriformis, hamstring, and lower back stretches. Strengthening exercises for core and gluteal muscles help support proper biomechanics.
Ergonomic adjustments at work and home can prevent recurrence. This may include using lumbar support cushions or adjusting desk and chair heights. Some patients benefit from periodic massage therapy or acupuncture.
Weight management plays a role in reducing pressure on the piriformis muscle. A balanced diet and regular low-impact cardiovascular exercise are recommended. Swimming and cycling are often well-tolerated activities.
Patients should be vigilant for any recurring symptoms. Early intervention with physical therapy or anti-inflammatory measures can prevent progression. Some individuals may require periodic cortisone injections for long-term management.
Frequently Asked Questions
What is the typical recovery time after piriformis release surgery?
Recovery time after piriformis release surgery typically ranges from 4-6 weeks. Most patients can resume light activities within 2 weeks. Full recovery and return to strenuous activities may take 2-3 months.
Physical therapy is an important part of the recovery process. Patients usually start gentle exercises and stretches within days of surgery to promote healing and restore function.
How much does piriformis syndrome surgery typically cost?
The cost of piriformis syndrome surgery can vary widely depending on location, surgeon, and facility. Without insurance, the procedure may cost between $5,000 to $30,000.
Insurance coverage can significantly reduce out-of-pocket expenses. Patients should check with their insurance provider regarding coverage and potential copays or deductibles.
What are the success rates associated with piriformis syndrome surgery?
Success rates for piriformis syndrome surgery are generally high, with many studies reporting 70-90% of patients experiencing significant pain relief. Individual results can vary based on factors like the severity of the condition and adherence to post-operative care.
Some patients may experience partial relief or recurrence of symptoms over time. Long-term success often depends on continued physical therapy and lifestyle modifications.
Are there any side effects associated with piriformis release surgery?
Potential side effects of piriformis release surgery include:
- Temporary pain and swelling at the surgical site
- Infection (rare)
- Bleeding or hematoma formation
- Nerve injury (uncommon)
- Muscle weakness
Most side effects are temporary and resolve with proper care. Serious complications are rare when the procedure is performed by an experienced surgeon.
Under what circumstances is piriformis syndrome surgery considered necessary?
Surgery for piriformis syndrome is typically considered when:
- Conservative treatments have failed after several months
- Symptoms are severe and significantly impact quality of life
- Imaging studies confirm compression of the sciatic nerve
- The patient has persistent pain or neurological symptoms
A thorough evaluation by a specialist is crucial to determine if surgery is appropriate.
How can one find a reputable clinic that performs piriformis syndrome surgery?
To find a reputable clinic for piriformis syndrome surgery:
- Research surgeons specializing in peripheral nerve disorders or orthopedic surgery
- Check surgeon credentials, experience, and patient reviews
- Consult with primary care physicians for recommendations
- Contact major medical centers or university hospitals in your area
It’s important to choose a surgeon with specific experience in piriformis release procedures. Don’t hesitate to ask about their success rates and complication rates.
