Migraine Surgery
- Miami -
Overview
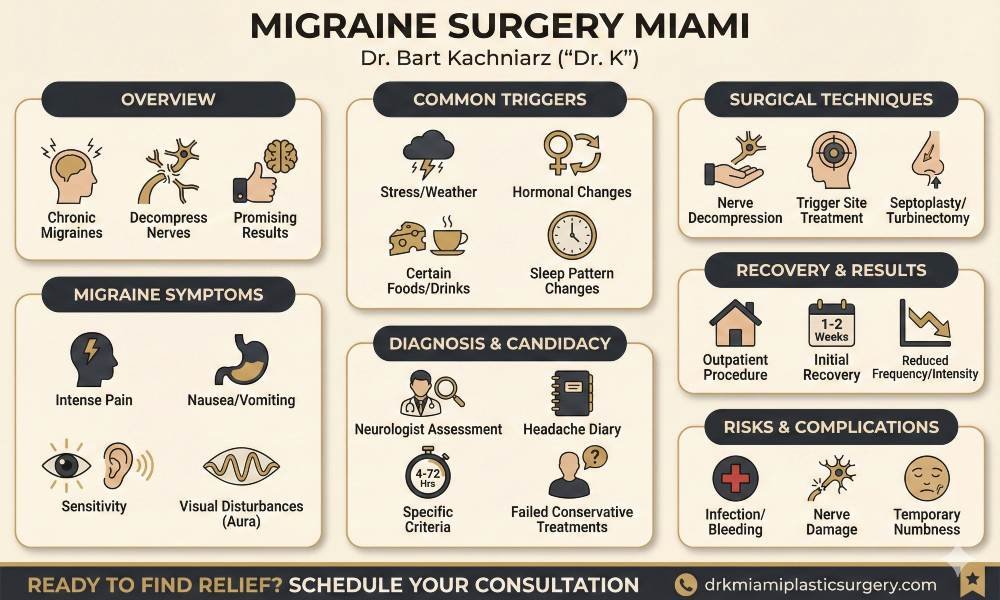
Migraine surgery offers a potential solution for those suffering from chronic migraines who have not found relief through traditional treatments. This surgical procedure aims to decompress specific nerves in the head and neck that may trigger migraine symptoms. Nerve decompression surgery has shown promising results for some patients, with success rates reported in various studies.
It’s important to note that migraine surgery is not a one-size-fits-all solution. Potential complications and varying success rates make it crucial for patients to thoroughly discuss the procedure with their healthcare providers. As with any surgical intervention, a thorough evaluation and understanding of the risks and benefits are essential before proceeding with migraine surgery.
Dr K Miami offers a consultations to patients that are looking for migraine solutions. Get in touch to see what your options are.


Understanding Migraine and Its Symptoms
Migraine attacks involve changes in brain activity and blood flow. The trigeminal nerve becomes activated, releasing inflammatory substances around blood vessels in the brain. This process can cause intense pain and other symptoms. Researchers believe that migraine sufferers may have a more sensitive nervous system that reacts strongly to certain stimuli.
Serotonin levels in the brain also play a role. During a migraine, these levels drop, which may contribute to the pain and other symptoms. Genetic factors can make some individuals more susceptible to migraines.
Identifying Common Migraine Triggers
Many factors can trigger migraines. Common triggers include:
- Stress and anxiety
- Hormonal changes, especially in women
- Certain foods and drinks (e.g., alcohol, caffeine, aged cheeses)
- Changes in sleep patterns
- Bright lights or loud noises
- Weather changes
Keeping a migraine diary can help identify personal triggers. This involves recording details about each attack, including potential triggers, symptoms, and duration.
Recognizing Migraine Symptoms
Migraine symptoms often extend beyond head pain. Common symptoms include:
- Intense, throbbing pain, usually on one side of the head
- Nausea and vomiting
- Sensitivity to light, sound, and sometimes smells
- Visual disturbances (aura) in some cases
- Dizziness or vertigo
Some people experience a prodrome phase before the headache, with symptoms like mood changes, food cravings, or neck stiffness. After the headache, a postdrome phase may occur, characterized by fatigue and difficulty concentrating.
Symptoms can vary between individuals and even between attacks in the same person. The duration of a migraine attack can range from a few hours to several days.
Conventional Migraine Treatments
Medications play a crucial role in managing migraines. Acute treatments, taken at the onset of symptoms, include over-the-counter pain relievers and prescription drugs like triptans. These medications work to alleviate pain and associated symptoms.
Preventive medications are taken regularly to reduce migraine frequency. Common options include:
- Beta-blockers
- Anticonvulsants
- Calcium channel blockers
- Tricyclic antidepressants
Doctors often prescribe these medications based on individual patient needs and potential side effects. Regular follow-ups help assess medication effectiveness and adjust dosages as needed.
Botox Injections and Migraine
Botox (onabotulinumtoxinA) injections have emerged as an effective treatment for chronic migraines. This approach involves injecting small amounts of Botox into specific head and neck muscles.
The procedure typically includes 31 injections in seven key areas. Patients usually receive treatments every 12 weeks. Botox works by blocking neurotransmitters that carry pain signals to the brain.
Studies show Botox can significantly reduce migraine days for many patients. Side effects are generally mild and may include neck pain or muscle weakness.
Neurological Approaches to Migraine
Neurologists play a vital role in migraine management, offering specialized diagnostic and treatment options. They may employ various techniques to address migraine symptoms:
- Nerve blocks: Injecting anesthetic near specific nerves to reduce pain
- Transcranial magnetic stimulation (TMS): Using magnetic pulses to stimulate the brain
- Biofeedback: Teaching patients to control certain bodily processes
Neurologists also help identify and manage migraine triggers. They may recommend lifestyle changes, such as stress reduction techniques or dietary modifications, to complement other treatments.
Advanced imaging techniques like MRI or CT scans may be used to rule out other neurological conditions and ensure accurate diagnosis.


Meet Your Doctor
With years of experience in the field of plastic surgery, Dr. K has built a reputation as one of Miami’s premier plastic surgeons.
His journey into medicine began with a passion for helping others and a keen eye for detail—qualities that have defined his career ever since, but what truly sets him apart is his genuine care for each patient who walks through our doors.
SEE WHAT WE CAN DO FOR YOU
Diagnosis and Referral Process
A neurologist plays a key role in evaluating patients with suspected migraine headaches. They conduct a thorough medical history and neurological examination. The neurologist may order imaging studies like MRI or CT scans to rule out other conditions.
Patients typically keep a headache diary to track frequency, duration, and severity of attacks. This information helps the neurologist assess the impact on daily life and determine if current treatments are effective.
If conventional therapies fail to provide adequate relief, the neurologist may refer suitable candidates to a migraine surgeon for further evaluation.

Migraine Diagnosis Criteria
Migraine diagnosis relies on specific criteria outlined in the International Classification of Headache Disorders (ICHD). Key diagnostic features include:
- Recurring headaches lasting 4-72 hours
- At least two of: unilateral location, pulsating quality, moderate to severe pain, aggravation by routine physical activity
- At least one of: nausea/vomiting, photophobia and phonophobia
A minimum of five attacks meeting these criteria is required for a definitive migraine diagnosis. The neurologist carefully evaluates symptoms to differentiate migraines from other headache disorders.
When to Consider Surgery
Migraine surgery is typically considered when:
- Conservative treatments have failed to provide adequate relief
- Headaches significantly impact quality of life
- Specific trigger sites can be identified
- The patient has realistic expectations about surgical outcomes
Candidates should have tried preventive medications and lifestyle modifications without success. Chronic migraine sufferers (15+ headache days per month) are often suitable surgical candidates.
A comprehensive evaluation by both a neurologist and migraine surgeon is essential to determine if surgery is appropriate. This team approach ensures patients receive the most suitable treatment for their individual situation.
Migraine Surgery Overview
Migraine surgery encompasses several techniques tailored to individual patient needs. The most common type is nerve decompression surgery, which focuses on releasing pressure on specific nerves around the head and neck. Another approach is trigger site deactivation, targeting areas known to initiate migraines.
Some surgeons perform arterial ligation, addressing blood vessels that may contribute to headaches. In certain cases, septoplasty or sinus surgery may be recommended if structural issues are identified as migraine triggers.
Each surgical method is selected based on a patient’s unique migraine patterns and trigger points identified through careful evaluation.
Understanding Nerve Decompression
Nerve decompression surgery is based on the theory that migraine pain often results from compressed nerves in the head and neck region. This procedure involves carefully removing small sections of tissue or bone that may be pressing on specific nerves.
Common target areas include:
- Frontal region (supraorbital and supratrochlear nerves)
- Temporal region (zygomaticotemporal nerve)
- Occipital region (greater occipital nerve)
During the procedure, surgeons use specialized techniques to release the affected nerves, aiming to reduce irritation and subsequent migraine triggers. The surgery is typically performed on an outpatient basis under general anesthesia.

Potential Benefits of Migraine Surgery
Migraine surgery offers several potential advantages for chronic sufferers. Many patients report a significant reduction in headache frequency and intensity following the procedure. Some individuals experience complete elimination of migraines.
Additional benefits may include:
- Decreased reliance on medication
- Improved quality of life
- Enhanced work productivity
- Reduced healthcare costs over time
It’s important to note that results can vary, and not all patients achieve the same level of improvement. Success rates are generally higher for carefully selected candidates who have undergone thorough evaluation and have identifiable trigger points.
Patients should discuss potential risks and benefits with their healthcare provider to determine if migraine surgery is an appropriate option for their specific situation.

Surgical Intervention Techniques
1. Nerve Decompression Technique
Nerve decompression surgery focuses on releasing compressed peripheral nerves that may contribute to migraine pain. Surgeons identify and free nerves from surrounding tissues that cause irritation or compression. Common sites include the supraorbital, supratrochlear, and occipital nerves.
The procedure typically involves making small incisions near the affected nerves. Surgeons then carefully dissect the area to remove muscle, fascia, or other structures impinging on the nerve. In some cases, they may perform a partial myectomy to reduce pressure.
Nerve decompression aims to reduce the frequency and intensity of migraine attacks by alleviating nerve irritation. This technique is often tailored to each patient’s specific trigger points and pain patterns.
2. Trigger Site Identification and Treatment
Trigger site surgery targets specific areas known to initiate migraine headaches. Surgeons first identify these sites through a combination of patient history, physical examination, and response to nerve blocks.
Common trigger points include:
- Frontal region (supraorbital and supratrochlear nerves)
- Temporal region (zygomaticotemporal nerve)
- Occipital region (greater and lesser occipital nerves)
- Nasal area (deviated septum or enlarged turbinates)
Treatment may involve deactivating trigger points through various means:
- Surgical release of muscular bands
- Removal of small sensory nerve branches
- Correction of anatomical irregularities
These interventions aim to reduce the activation of migraine pathways and decrease headache frequency.
3. Septoplasty and Turbinectomy Procedures
Nasal surgery can be an effective intervention for patients with migraines triggered by intranasal abnormalities. Septoplasty involves correcting a deviated nasal septum, which can cause contact points within the nose and trigger headaches.
The procedure straightens the septum, reducing nasal obstruction and potential trigger points. Surgeons may also perform a turbinectomy to reduce the size of enlarged turbinates, further improving nasal airflow and reducing pressure points.
These nasal procedures can be particularly beneficial for patients with migraines associated with sinus pressure or those experiencing relief from nasal sprays. By addressing anatomical issues, surgeons aim to eliminate nasal trigger points and improve overall nasal function.
Assessing Candidacy for Surgery
Ideal candidates for migraine surgery have chronic migraines that are refractory to conservative treatments. Patients should have a confirmed diagnosis from a neurologist and documented failure of conventional therapies. Trigger point identification is crucial, typically done through nerve blocks or botulinum toxin injections.
Age, overall health status, and comorbidities play a role in candidacy. Psychological evaluation may be necessary to assess pain coping mechanisms and expectations. Patients with unrealistic expectations or secondary gain issues may not be suitable candidates.
Imaging studies, such as MRI or CT scans, are often performed to rule out structural abnormalities. These tests help ensure that symptoms are not caused by underlying conditions requiring different interventions.
Understanding the Risks and Complications
Migraine surgery, like any surgical procedure, carries inherent risks. Potential complications include:
- Infection
- Bleeding
- Nerve damage
- Scarring
- Anesthesia-related issues
- Temporary or permanent numbness
- Muscle weakness
Patients may experience a lack of improvement or worsening of symptoms in some cases. The possibility of developing new pain patterns or migraine triggers should be discussed.
Surgeons must thoroughly explain these risks to patients. Informed consent is crucial, ensuring patients understand potential outcomes and complications before proceeding with surgery.
Preparing for Surgery
Preoperative preparation involves several steps:
- Medical clearance from primary care physician
- Discontinuation of certain medications (e.g., blood thinners)
- Fasting guidelines before surgery
- Arranging transportation and post-operative care
Patients should optimize their health by:
- Quitting smoking
- Maintaining a healthy diet
- Staying hydrated
- Getting adequate rest
Surgeons may recommend specific relaxation techniques or stress reduction methods to help manage anxiety before the procedure. Patients should also prepare their home environment for a comfortable recovery period.
Clear communication about post-operative expectations, including pain management and activity restrictions, is essential. This helps patients plan for their recovery and set realistic goals for improvement.
Recovery and Downtime Expectations
Most migraine surgeries are performed on an outpatient basis. Patients typically return home the same day. The initial recovery period lasts about 1-2 weeks.
Swelling and bruising around the surgical sites are common. These symptoms usually peak within 48-72 hours after surgery and gradually subside.
Patients may experience temporary numbness or itching in the treated areas. These sensations are normal and should resolve as healing progresses.
Light activities can often be resumed within a few days. However, strenuous exercise should be avoided for 2-4 weeks.
Full recovery may take several weeks to months, depending on the extent of the surgery and individual healing rates.
Long-term Results and Efficacy
Migraine surgery aims to reduce headache frequency and intensity. Results can vary among patients.
Many individuals report significant improvement within 3-6 months post-surgery. Some experience immediate relief, while others may see gradual changes over time.
Studies show that 70-90% of patients experience a reduction in migraine frequency or severity after surgery.
Complete elimination of migraines is not guaranteed. Some patients may still require medication for breakthrough headaches.
Long-term success rates are generally positive, with many patients maintaining improvements for years after the procedure.
Handling Complications and Side Effects
While rare, potential complications include infection, bleeding, or adverse reactions to anesthesia. Patients should promptly report any unusual symptoms to their surgeon.
Some individuals may experience temporary hair loss near incision sites. This is usually temporary and resolves within a few months.
Persistent numbness or changes in sensation can occur in treated areas. These effects often improve with time but may be permanent in some cases.
Rarely, patients may notice changes in facial expressions or muscle movement. If this occurs, follow-up with the surgeon is essential.
Managing expectations and maintaining open communication with the healthcare team are crucial for addressing any postoperative concerns effectively.
Finding a Specialized Surgeon
Locating a qualified surgeon experienced in migraine procedures is crucial. Patients can start by consulting their neurologist or primary care physician for referrals. Many plastic surgeons now specialize in migraine surgery techniques.
Professional medical associations often maintain directories of surgeons with specific expertise. Online resources and patient forums can also provide recommendations and reviews of surgeons who perform migraine procedures.
It’s important to research potential surgeons’ credentials, experience, and success rates. Patients should seek consultations with multiple specialists to discuss treatment options and surgical approaches.
