Peripheral Nerve Surgery
- Miami -
overview
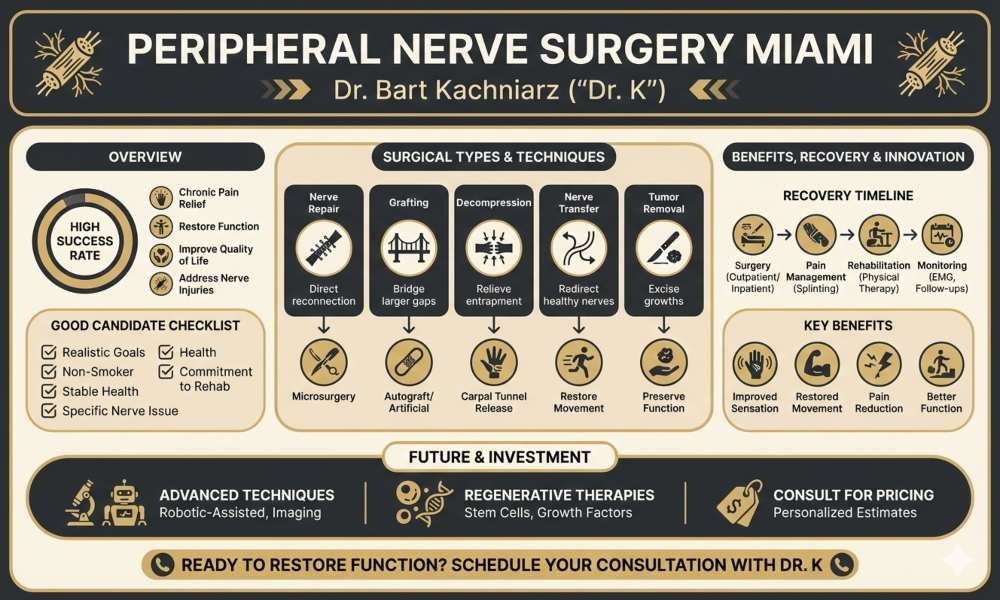
Peripheral nerve surgery offers hope for patients suffering from chronic pain, nerve injuries, and conditions like carpal tunnel syndrome. This specialized field focuses on repairing and regenerating damaged nerves to restore function and sensation. Surgical interventions can significantly improve quality of life for those who have not found relief through conservative treatments.
Peripheral nerve surgeries encompass a range of procedures tailored to specific nerve issues. These may include nerve decompression, repair of severed nerves, or removal of nerve tumors. Advanced techniques such as nerve grafting and nerve transfers have expanded treatment options, allowing surgeons to address complex cases with improved outcomes.
Patients considering peripheral nerve surgery undergo thorough evaluations to determine the best course of action.While surgery can be transformative, it is often considered after non-invasive treatments have been exhausted, balancing potential benefits against surgical risks. Get in touch with Dr K and see if surgery is right for you.


Understanding Peripheral Nerves and Nerve Injuries
Peripheral nerves consist of bundles of nerve fibers encased in protective tissue. They include motor nerves, which control muscles, and sensory nerves, which relay information about touch, temperature, and pain.
The structure of a peripheral nerve includes:
- Axons: Long, slender projections of nerve cells
- Myelin sheath: Insulating layer around axons
- Endoneurium: Connective tissue surrounding individual nerve fibers
- Perineurium: Protective layer enclosing bundles of nerve fibers
- Epineurium: Outermost protective sheath of the entire nerve
This complex anatomy allows for efficient signal transmission and helps protect the delicate nerve fibers from injury.
Common Types of Nerve Injuries
Nerve injuries can occur through various mechanisms:
- Compression: Prolonged pressure on a nerve, as in carpal tunnel syndrome
- Stretch: Forceful elongation of a nerve beyond its normal range
- Laceration: Cutting or tearing of nerve fibers
- Ischemia: Reduced blood supply to the nerve
Injuries are classified based on severity:
- Neuropraxia: Temporary loss of function without structural damage
- Axonotmesis: Damage to axons with intact supportive structures
- Neurotmesis: Complete severance of the nerve
Symptoms and Diagnosis of Nerve Damage
peripheral nerve injuries vary depending on the affected nerve and severity of damage. Common signs include:
- Numbness or tingling sensations
- Weakness or paralysis in affected muscles
- Burning or shooting pain
- Loss of sensation in the affected area
Diagnosis typically involves:
- Physical examination
- Neurological tests to assess muscle strength and sensation
- Electromyography (EMG) to evaluate muscle function
- Nerve conduction studies to measure nerve signal transmission
Advanced imaging techniques such as MRI or ultrasound may be used to visualize nerve damage and surrounding structures. These diagnostic tools help determine the extent of injury and guide treatment decisions.
Types of Peripheral Nerve Surgeries
Nerve Repair and Grafting
Nerve repair surgery restores continuity to severed or damaged nerves. Surgeons use microsurgical techniques to reconnect nerve endings, enabling regrowth and regeneration. For larger gaps, nerve grafting may be necessary.
Grafts can be autologous (from the patient’s own body) or artificial. Autologous grafts often come from sensory nerves in less critical areas. Artificial grafts use biocompatible materials to bridge nerve gaps.
The success of nerve repair depends on factors like injury severity, timing of surgery, and the specific nerve involved. Recovery can take months or even years as nerves regenerate slowly.
Tumor Removal
Peripheral nerve tumors, such as schwannomas and neurofibromas, can cause pain, weakness, or numbness. Surgical removal is often the primary treatment option.
Schwannomas are typically benign and encapsulated, making them easier to remove without damaging the nerve. Neurofibromas, however, may intertwine with nerve fibers, requiring more delicate dissection.
Surgeons use microsurgical techniques to carefully separate the tumor from healthy nerve tissue. In some cases, partial nerve resection may be necessary, followed by nerve grafting or transfer.
Decompression Procedures
Nerve entrapment syndromes occur when nerves are compressed, leading to pain, numbness, or weakness. Decompression surgeries aim to relieve this pressure and restore normal nerve function.
Common decompression procedures include:
- Carpal tunnel release for median nerve compression in the wrist
- Cubital tunnel release for ulnar nerve compression at the elbow
- Tarsal tunnel release for tibial nerve compression in the ankle
- Peroneal nerve decompression at the knee
These surgeries involve cutting through tight ligaments or fascia to create more space for the affected nerve. Many can be performed as outpatient procedures with minimal recovery time.
Nerve Transfer
Nerve transfer surgery redirects healthy nerves to restore function in areas affected by nerve damage. This technique is particularly useful when the original nerve is irreparable or when time is critical for muscle reinnervation.
Surgeons identify expendable donor nerves near the affected area. They then reroute these nerves to connect with the distal portion of the damaged nerve or directly to target muscles.
Nerve transfers can restore various functions, including:
- Elbow flexion in brachial plexus injuries
- Hand function after spinal cord injuries
- Facial reanimation in facial nerve palsy
Recovery requires extensive rehabilitation as the brain adapts to new nerve pathways. Results can be significant, often surpassing those of traditional nerve grafting in certain cases.


Meet Your Doctor
With years of experience in the field of plastic surgery, Dr. K has built a reputation as one of Miami’s premier plastic surgeons.
His journey into medicine began with a passion for helping others and a keen eye for detail—qualities that have defined his career ever since, but what truly sets him apart is his genuine care for each patient who walks through our doors.
SEE WHAT WE CAN DO FOR YOU
Preoperative Considerations
Consultation
Patients should consult with a multidisciplinary team at a specialized peripheral nerve surgery center. This team typically includes neurosurgeons, neurologists, and physical medicine and rehabilitation specialists.
Each expert contributes unique insights to develop an optimal treatment plan. Neurosurgeons evaluate surgical options and techniques. Neurologists assess nerve function and potential for recovery.
Physical medicine specialists recommend pre- and post-operative rehabilitation strategies. This collaborative approach ensures all aspects of the patient’s condition are considered before proceeding with surgery.

Medical History Review
A detailed medical history review is essential. The specialist team examines past injuries, surgeries, and chronic conditions that may impact nerve health or surgical outcomes.
Physical examination includes:
- Strength testing
- Sensory assessments
- Range of motion evaluation
- Nerve conduction studies
These tests help pinpoint the exact location and severity of nerve damage. Imaging studies like MRI or ultrasound may be ordered to visualize affected nerves and surrounding structures.
Preexisting medical conditions such as diabetes or autoimmune disorders require careful consideration, as they can affect nerve healing and surgical risks.
Surgical Intervention
Open surgery remains a cornerstone of peripheral nerve repair. Neurosurgeons access the affected nerve through an incision, allowing direct visualization and manipulation. This approach is crucial for complex cases requiring extensive repair or reconstruction.
Microsurgical techniques are employed to reconnect severed nerves with precision. Surgeons use specialized instruments and microscopes to align and suture nerve endings. For larger gaps, nerve grafts may be harvested from elsewhere in the body to bridge the defect.
Nerve decompression is another common procedure. It involves releasing compressed nerves from surrounding tissues, often seen in conditions like carpal tunnel syndrome.

Minimally Invasive and Endoscopic Techniques
Advancements in technology have led to less invasive surgical options. Endoscopic approaches use small incisions and cameras to access and treat peripheral nerves.
These techniques are particularly useful for nerve decompressions. They result in smaller scars, less tissue damage, and potentially faster recovery times compared to open surgery.
Ultrasound-guided procedures allow surgeons to target specific nerves for interventions like nerve blocks or electrical stimulation. This precision helps in both diagnosis and treatment of nerve disorders.
Advanced Nerve Reconstruction
Nerve transfers represent a significant advancement in peripheral nerve surgery. This technique involves rerouting healthy nerves to restore function in areas with irreparable nerve damage.
Nerve conduits and allografts provide alternatives to autografts for bridging nerve gaps. These synthetic or processed materials can guide nerve regeneration without the need for harvesting the patient’s own nerves.
Neurostimulation devices may be implanted to modulate nerve activity and manage chronic pain. These systems deliver electrical impulses to specific nerves, offering relief when other treatments have failed.
Postoperative Care
Pain management is a top priority immediately after surgery. Physicians may prescribe analgesics or utilize nerve block catheters to provide targeted pain relief. Early mobilization is encouraged to promote neural gliding and prevent adhesions.
Patients receive instructions on wound care and how to protect the surgical site. Depending on the procedure, temporary immobilization may be necessary. However, prolonged splinting is generally avoided to prevent joint stiffness.
Careful monitoring for signs of infection or complications is essential during this phase. Patients are educated on recognizing potential issues and when to seek medical attention.
Long-term Rehabilitation and Physical Therapy
As healing progresses, the focus shifts to rehabilitation. Physical therapy plays a crucial role in restoring function and improving outcomes. A tailored program is designed to:
- Increase range of motion
- Enhance muscle strength
- Improve coordination
- Prevent contractures
Therapists may employ various techniques such as:
- Gentle stretching exercises
- Electrical stimulation
- Massage therapy
- Specific movement patterns to encourage nerve regeneration
Patients are taught home exercises to complement in-clinic sessions. The rehabilitation process can be lengthy, often lasting several months to a year, depending on the extent of nerve damage.
Monitoring for Complications and Success
Regular follow-up appointments with surgeons and neurologists are essential to track recovery progress. These visits may include:
- Physical examinations
- Strength and sensation tests
- Electromyography (EMG) studies to assess nerve function
Physicians monitor for potential complications such as:
- Neuroma formation
- Persistent pain
- Inadequate nerve regeneration
Success is measured by improvements in:
- Pain reduction
- Return of sensation
- Muscle strength gains
- Functional abilities in daily activities
Adjustments to the treatment plan are made as needed based on progress. Patient education continues throughout this phase, ensuring realistic expectations and promoting adherence to the rehabilitation program.

Measuring Surgical Success
Surgical success is evaluated through multiple methods. Sensory and motor function tests assess nerve regeneration progress. Two-point discrimination tests measure tactile sensitivity. Muscle strength grading helps quantify motor recovery.
Electromyography (EMG) and nerve conduction studies provide objective data on reinnervation. These tests can detect early signs of nerve regrowth before clinical improvements are apparent.
Imaging techniques like ultrasound and MRI aid in visualizing nerve repair and monitoring for complications. They can reveal nerve continuity, swelling, or scar tissue formation.
Potential for Nerve Regeneration
Nerve regeneration potential depends on several factors. The type and location of injury significantly impact recovery. Proximal injuries generally have poorer outcomes due to longer regeneration distances.
Timing of surgery is crucial. Early intervention often yields better results, as prolonged denervation can lead to irreversible muscle atrophy. Nerves typically regenerate at a rate of 1-3 mm per day.
Age plays a role in recovery potential. Younger patients tend to have better regenerative capacity and functional outcomes. Comorbidities like diabetes can impair nerve healing and regrowth.
Non-Surgical Treatments and Therapies
Pharmacological Interventions
Medications form an essential component of non-surgical treatment for peripheral nerve injuries. Nonsteroidal anti-inflammatory drugs (NSAIDs) help reduce pain and inflammation. Gabapentin and pregabalin are commonly prescribed to manage neuropathic pain.
Corticosteroids may be used in some cases to decrease inflammation and swelling around the injured nerve. Vitamins, particularly B-complex vitamins, are often recommended to support nerve health and regeneration.
In certain situations, topical treatments like lidocaine patches or capsaicin cream can provide localized pain relief. Ongoing clinical trials are exploring innovative medications to enhance nerve repair and regeneration.
Physical Therapy and Rehabilitation
Physical therapy is a cornerstone of non-surgical treatment for peripheral nerve injuries. Therapists design tailored exercise programs to maintain muscle strength, prevent joint stiffness, and improve range of motion.
Specific exercises focus on:
- Strengthening affected muscles
- Improving coordination and balance
- Enhancing sensory function
Therapists may employ techniques such as:
- Electrical stimulation to activate muscles
- Ultrasound therapy to reduce pain and promote healing
- Manual therapy to improve circulation and reduce scar tissue
Rehabilitation programs often incorporate occupational therapy to help patients regain independence in daily activities. Regular exercise under professional guidance is crucial for optimal recovery.
Splints, Braces, and Assistive Devices
Orthotic devices play a vital role in supporting and protecting injured nerves during the healing process. Splints and braces help maintain proper limb position, preventing further damage and promoting optimal nerve function.
Common applications include:
- Wrist splints for carpal tunnel syndrome
- Ankle-foot orthoses for foot drop
- Elbow braces for ulnar nerve compression
These devices are often custom-fitted to ensure comfort and effectiveness. Assistive devices like modified utensils or grab bars may be recommended to aid in daily activities during recovery.
Regular adjustments and follow-ups with healthcare providers ensure that these devices continue to meet the patient’s evolving needs throughout the healing process.
Innovations in Nerve Surgery
Novel surgical techniques are emerging to enhance nerve repair and regeneration. Microsurgical advancements allow for more precise interventions, improving the chances of successful nerve reconnection. Bioengineered nerve grafts show promise in bridging larger nerve gaps, potentially reducing the need for autografts.
Stem cell therapies are being explored to promote nerve regeneration. Clinical trials are investigating the use of mesenchymal stem cells to support nerve growth and functional recovery. These innovative approaches may lead to faster healing and better long-term outcomes for patients with peripheral nerve injuries.
Genetic and Molecular Research
Genetic studies are uncovering the molecular mechanisms behind nerve regeneration. This knowledge is paving the way for targeted therapies to enhance nerve repair. Researchers are investigating gene therapies to boost the expression of growth factors crucial for nerve regeneration.
Molecular research is also focusing on developing new pharmacological agents to support nerve healing. These drugs may help reduce scar tissue formation and promote a more conducive environment for nerve regrowth. As our understanding of the genetic basis of peripheral nerve disorders deepens, personalized treatment strategies may become a reality.
The Future of Peripheral Nerve Surgery
Advanced imaging techniques are revolutionizing peripheral nerve surgery. High-resolution ultrasound and MRI scans allow surgeons to visualize nerve structures in unprecedented detail. This improved imaging helps in precise diagnosis and surgical planning.
Robotic-assisted microsurgery is gaining traction, offering enhanced precision and stability during delicate nerve procedures. Virtual reality simulations are being used for surgical training and planning complex cases. 3D-printed nerve guides and scaffolds are being developed to support nerve regeneration in customized ways.
Wearable technology and smart prosthetics integrated with peripheral nerve interfaces are advancing rapidly. These innovations may provide improved sensory feedback and motor control for patients with nerve injuries or amputations.
Frequently Asked Questions
How much does peripheral nerve surgery typically cost?
Costs vary widely based on the specific procedure, location, and insurance coverage. Simple nerve repairs may cost several thousand dollars, while complex reconstructions can exceed $50,000. Patients should consult their insurance provider and surgeon for accurate estimates.
What is the expected recovery time following peripheral nerve surgery?
Recovery times differ depending on the surgery type and extent of nerve damage. Minor procedures may allow return to activities within weeks. Major reconstructions often require months of rehabilitation. Nerve regeneration occurs slowly, at about 1 mm per day.
Which surgical options are available for neuropathy in the feet?
Surgical options for foot neuropathy include nerve decompression, which releases pressure on affected nerves. Nerve transfers can restore function in some cases. Surgeons may also perform neurolysis to free nerves from scar tissue.
How can peripheral nerve damage be repaired surgically?
Surgeons can directly repair severed nerves by reconnecting the ends. For larger gaps, nerve grafts from other body areas may be used. Nerve transfers redirect functioning nerves to restore movement or sensation in the affected area.
