Nerve Compression Syndrome
-Miami-
Overview
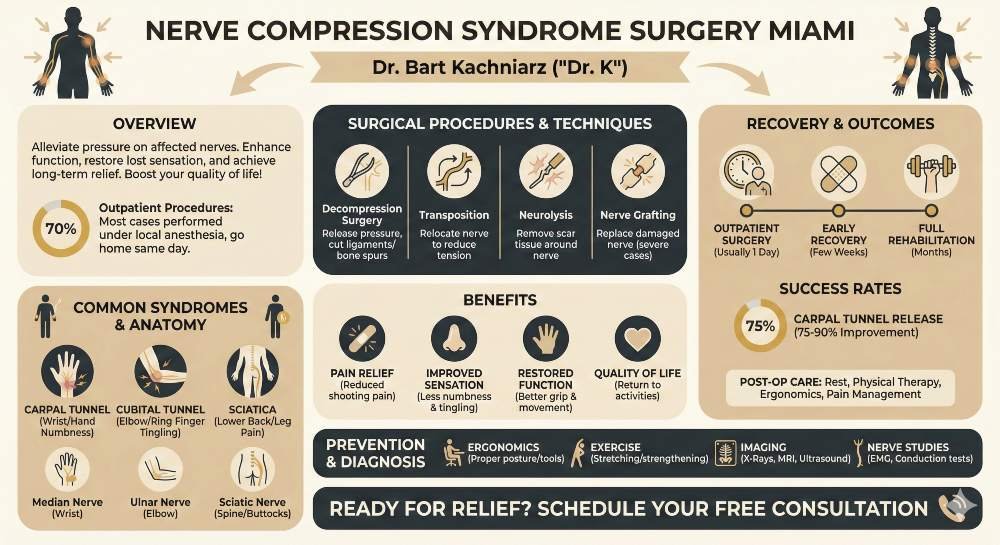
Nerve compression syndrome occurs when a nerve is squeezed or compressed, causing pain, numbness, and other symptoms. This condition can affect various parts of the body, including the hands, wrists, elbows, and feet. When conservative treatments fail to provide relief, surgery may be necessary.
Nerve compression syndrome surgery aims to alleviate pressure on the affected nerve by increasing the size of the surrounding space or removing structures that are causing compression. These procedures are typically performed on an outpatient basis under local anesthesia, allowing patients to return home the same day. In some cases, general anesthesia may be recommended.
Surgical intervention can effectively treat conditions such as carpal tunnel syndrome, cubital tunnel syndrome, and tarsal tunnel syndrome. See if surgery is an option for you by contacting us at Dr K Miami and get a free consultation with Dr Bart Kachniraz and explore what your options are.


Understanding Nerve Compression Syndromes
Nerve compression syndromes involve pressure on specific nerves, leading to dysfunction. Common types include carpal tunnel syndrome, cubital tunnel syndrome, and sciatica.
Carpal tunnel syndrome affects the median nerve in the wrist, causing hand and finger numbness. Cubital tunnel syndrome impacts the ulnar nerve at the elbow, resulting in tingling in the ring and little fingers.
Sciatica involves compression of the sciatic nerve, causing lower back and leg pain. Radial nerve compression can occur in the arm, leading to wrist and hand weakness.
Common Causes
eral factors can contribute to nerve compression syndromes:
- Repetitive motions or overuse injuries
- Trauma or accidents
- Arthritis and joint inflammation
- Bone spurs or herniated disks
- Diabetes
- Dislocated joints
- Tissue swelling
Work-related activities, such as typing or using vibrating tools, can increase the risk of developing these conditions. Maintaining poor posture or sleeping in awkward positions may also contribute to nerve compression.
Anatomy of Nerve Compression
Nerve compression typically occurs at specific anatomical points where nerves pass through narrow spaces. These areas are vulnerable to pressure from surrounding tissues.
In carpal tunnel syndrome, the median nerve is compressed as it passes through the carpal tunnel in the wrist. The ulnar nerve is susceptible to compression at the elbow in cubital tunnel syndrome.
The sciatic nerve can be compressed as it exits the spine or travels through the buttocks. Radial nerve compression often occurs in the upper arm, where the nerve wraps around the humerus bone.
Understanding the anatomy of these compression points is crucial for diagnosis and treatment planning.
Symptoms of Nerve Compression
Pain is a primary indicator of nerve compression. It can range from mild discomfort to severe, shooting pain along the affected nerve’s path. Numbness and tingling sensations, known as paresthesias, frequently accompany nerve compression. These sensations may occur in specific areas served by the compressed nerve.
Muscle weakness is another common symptom. Patients may experience difficulty performing certain movements or notice a decrease in grip strength. In some cases, muscle atrophy can occur if compression persists for an extended period.
Sensitivity to touch in the affected area may increase. Some individuals report a burning sensation or a feeling of “pins and needles.”
Specific Syndromes
Carpal tunnel syndrome, a well-known nerve compression condition, typically causes pain, numbness, and tingling in the hand and fingers. Patients often report worsening symptoms at night or during repetitive hand movements.
Sciatica, resulting from compression of the sciatic nerve, leads to pain radiating from the lower back down the leg. Some individuals experience difficulty walking or standing for long periods.
Cervical radiculopathy, caused by nerve root compression in the neck, can produce pain, weakness, and numbness in the shoulders, arms, and hands. Patients may have trouble turning their head or experience headaches.
In severe cases of spinal cord compression, individuals may develop bladder or bowel incontinence. This requires immediate medical attention to prevent permanent nerve damage.
Diagnostic Procedures
Physical examination forms the cornerstone of diagnosing nerve compression syndromes. A neurologist or orthopedic specialist evaluates the patient’s symptoms and performs targeted tests.
They assess muscle strength, reflexes, and sensation in the affected area. Specific maneuvers may be used to reproduce symptoms, such as Tinel’s sign for carpal tunnel syndrome.
The physician examines posture, range of motion, and checks for visible swelling or deformities. A detailed medical history is taken, including occupational factors and previous injuries.
Imaging Techniques
Imaging studies provide valuable information about the structural causes of nerve compression. X-rays can reveal bone spurs or fractures that may be impinging on nerves.
Magnetic Resonance Imaging (MRI) offers detailed views of soft tissues, allowing visualization of nerve pathways and potential sources of compression. It can identify tumors, herniated discs, or inflamed tissues.
Ultrasound imaging is increasingly used for its real-time capabilities. It can show nerve swelling and surrounding tissue abnormalities. Ultrasound also aids in guiding injections for treatment.
Nerve Conduction Studies
Electrophysiological tests are crucial for assessing nerve function and locating areas of compression. Nerve conduction studies measure the speed and strength of electrical signals traveling through nerves.
Electrodes placed on the skin stimulate nerves and record their responses. Delayed or weakened signals indicate nerve damage or compression.
Electromyography (EMG) complements nerve conduction studies. It involves inserting thin needles into muscles to record electrical activity. This test helps differentiate between nerve and muscle disorders.
These studies can quantify the severity of nerve compression and track changes over time, aiding in treatment decisions and monitoring progress.


Meet Your Doctor
With years of experience in the field of plastic surgery, Dr. K has built a reputation as one of Miami’s premier plastic surgeons.
His journey into medicine began with a passion for helping others and a keen eye for detail—qualities that have defined his career ever since, but what truly sets him apart is his genuine care for each patient who walks through our doors.
SEE WHAT WE CAN DO FOR YOU
Non-Surgical Treatments
Pain relief medications play a crucial role in managing nerve compression symptoms. Nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen help reduce inflammation and alleviate pain. For more severe cases, doctors may prescribe stronger painkillers or muscle relaxants.
Corticosteroid injections can provide targeted relief. These injections deliver potent anti-inflammatory medication directly to the affected area, reducing swelling and alleviating pressure on the compressed nerve. The effects can last for several weeks to months.
Gabapentin or pregabalin, medications typically used for nerve pain, may be prescribed to address specific symptoms associated with nerve compression syndromes.

Physical Therapy
Physical therapy is a cornerstone of non-surgical treatment for nerve compression. A tailored exercise program can help strengthen muscles, improve flexibility, and enhance overall function. Therapists may use techniques such as:
- Stretching exercises to improve range of motion
- Strengthening exercises to support affected areas
- Manual therapy to mobilize soft tissues and joints
- Posture correction techniques
Physical therapists may also employ modalities like ultrasound or electrical stimulation to reduce pain and promote healing. They often teach patients proper body mechanics to prevent further nerve compression.
Lifestyle Modifications
Simple changes in daily habits can significantly impact nerve compression symptoms. These modifications may include:
- Ergonomic adjustments at work or home
- Weight management to reduce pressure on affected areas
- Proper posture and body mechanics during activities
- Regular breaks from repetitive tasks or prolonged positions
Patients are often advised to avoid activities that exacerbate symptoms. In some cases, temporary rest or activity modification may be recommended to allow the affected area to heal.

Splinting and Bracing
Splints and braces can provide support and limit movement in the affected area, reducing pressure on the compressed nerve. For example:
- Wrist splints for carpal tunnel syndrome
- Elbow braces for cubital tunnel syndrome
- Ankle braces for tarsal tunnel syndrome
These devices are often worn at night or during activities that trigger symptoms. They help maintain a neutral position, preventing further compression and allowing the nerve to heal.
Custom-fitted splints or braces may be prescribed for optimal support and comfort. Patients are typically instructed on proper use and duration to maximize benefits while avoiding dependency or muscle weakness.
Surgical Intervention
Surgery may be recommended when patients experience persistent pain, numbness, or weakness that does not respond to non-surgical treatments. Severe cases with muscle atrophy or significant functional impairment often require surgical intervention. Electrodiagnostic studies and imaging results can help determine the need for surgery.
Conditions such as carpal tunnel syndrome, cubital tunnel syndrome, and thoracic outlet syndrome may necessitate surgical treatment when symptoms become debilitating. The decision to proceed with surgery is typically made after careful evaluation of the patient’s symptoms, medical history, and response to conservative therapies.
Types of Surgical Procedures
Several surgical techniques are employed to address nerve compression syndromes:
- Decompression surgery: This involves releasing pressure on the affected nerve by cutting through tight ligaments or removing bone spurs.
- Transposition: The compressed nerve is moved to a new location to reduce tension and pressure.
- Neurolysis: Scar tissue around the nerve is removed to improve mobility and function.
- Nerve grafting: In severe cases, damaged nerve segments may be replaced with healthy nerve tissue.
Minimally invasive approaches, such as endoscopic techniques, are increasingly used to reduce surgical trauma and promote faster recovery.
Risks and Complications
As with any surgical procedure, nerve compression syndrome surgery carries certain risks:
- Infection
- Bleeding
- Anesthesia-related complications
- Nerve damage
- Persistent or worsening symptoms
- Scarring
Surgeons take precautions to minimize these risks, but patients should be aware of potential complications. The likelihood of complications varies depending on the specific procedure and individual patient factors.
Recovery and Rehabilitation
Post-operative recovery typically involves a period of rest followed by gradual resumption of activities. Pain management and wound care are essential in the early stages of recovery. Physical therapy often plays a crucial role in rehabilitation, helping patients regain strength and function.
Rehabilitation protocols may include:
- Range of motion exercises
- Strengthening exercises
- Nerve gliding techniques
- Ergonomic training
The duration of recovery varies depending on the procedure and individual healing rates. Patients are usually advised to avoid strenuous activities for several weeks to months after surgery.
Success Rates of Surgical Treatment
Success rates for nerve compression syndrome surgery vary depending on the specific condition and procedure. Many patients experience significant improvement in symptoms and function following surgery. For example, carpal tunnel release surgery has reported success rates of 75-90%.
Factors influencing surgical outcomes include:
- Severity and duration of symptoms before surgery
- Patient age and overall health
- Adherence to post-operative care instructions
- Presence of underlying medical conditions
While surgery can provide substantial relief, some patients may experience incomplete resolution of symptoms or recurrence over time. Long-term follow-up and ongoing management may be necessary to maintain optimal outcomes.
Special Considerations
Certain factors can significantly influence the development and treatment of nerve compression syndromes. These include medical conditions, physical attributes, life stages, and occupational hazards.
- Diabetes and Nerve Compression
Diabetes increases the risk of nerve compression syndromes. Elevated blood sugar levels can damage nerves, making them more susceptible to compression.
Diabetic patients often experience delayed healing after surgery. This can prolong recovery time and increase the risk of complications.
Strict blood sugar control is crucial before and after surgery. It helps optimize surgical outcomes and reduces the likelihood of postoperative infections.
Diabetic patients may require longer follow-up periods. Regular monitoring is essential to detect any signs of recurrence or new compression sites.
- Obesity and Its Impact
Excess weight puts additional pressure on nerves, particularly in the wrists and elbows. This increases the risk of developing carpal tunnel and cubital tunnel syndromes.
Weight loss can significantly improve symptoms in obese patients. It may even eliminate the need for surgical intervention in some cases.
Surgical procedures may be more challenging in obese patients. Deeper tissue layers and limited visibility can complicate the operation.
Post-operative recovery may be slower in obese individuals. They may require longer immobilization periods and more intensive physical therapy.
- Pregnancy-Related Nerve Compression
Pregnancy often exacerbates or triggers nerve compression syndromes. Hormonal changes and fluid retention contribute to increased pressure on nerves.
Carpal tunnel syndrome is particularly common during pregnancy. Symptoms often resolve after delivery, but may persist in some cases.
Conservative treatments are preferred during pregnancy. These include splinting, physical therapy, and lifestyle modifications.
Surgical intervention is typically postponed until after delivery. Emergency procedures may be necessary in severe cases with muscle weakness or atrophy.
- Occupational Risks
Certain occupations increase the risk of nerve compression syndromes. Construction workers, assembly line workers, and office workers are particularly susceptible.
Repetitive motions and prolonged awkward positions contribute to nerve compression. Proper ergonomics and regular breaks can help prevent these conditions.
Occupational therapy plays a crucial role in treatment. It focuses on modifying work techniques and environments to reduce stress on affected nerves.
Return-to-work protocols should be tailored to each patient’s occupation. Gradual reintroduction of work activities helps prevent symptom recurrence.
Associated Conditions
1. Rheumatoid Arthritis and Related Neuropathies
Rheumatoid arthritis (RA) frequently leads to nerve compression syndromes. The inflammation and joint deformities characteristic of RA can put pressure on nearby nerves. Carpal tunnel syndrome is particularly common in RA patients, affecting up to 23% of cases.
Peripheral neuropathy is another complication of RA. It can cause numbness, tingling, and weakness in the extremities. This neuropathy may result from nerve compression or direct damage to nerves from the inflammatory process.
Treatment for RA-related nerve compression often involves managing the underlying arthritis. This may include medications to reduce inflammation and slow joint damage. In severe cases, surgical intervention may be necessary to relieve pressure on affected nerves.
2. Herniated Discs and Spinal Stenosis
Herniated discs and spinal stenosis are frequent causes of nerve compression in the spine. A herniated disc occurs when the soft inner portion of an intervertebral disc protrudes through the tougher outer layer. This can put pressure on nearby nerves, causing radiculopathy.
Symptoms of disc herniation include:
- Pain radiating down the arm or leg
- Numbness or tingling in affected areas
- Muscle weakness
Spinal stenosis involves narrowing of the spinal canal, which can compress the spinal cord or nerve roots. It often affects the lumbar region, leading to sciatic nerve compression. Cervical stenosis can cause cervical radiculopathy.
Treatment options range from conservative measures like physical therapy to surgical interventions such as lumbar decompression surgery or discectomy.
3. Systemic Diseases Affecting Nerves
Several systemic diseases can contribute to nerve compression syndromes. Diabetes is a leading cause of peripheral neuropathy, which can increase susceptibility to nerve compression. Diabetic neuropathy affects up to 50% of people with diabetes.
Hypothyroidism can lead to fluid retention and swelling, potentially compressing nerves. It’s associated with an increased risk of carpal tunnel syndrome.
Osteoarthritis, while primarily affecting joints, can indirectly cause nerve compression through bone spurs or joint deformities. These changes can narrow nerve passages, leading to conditions like foraminal stenosis.
Management of these systemic conditions is crucial in preventing and treating associated nerve compression syndromes. This often involves a multidisciplinary approach, combining disease-specific treatments with targeted therapies for nerve compression.
Preventing Nerve Compression
Proper ergonomics play a crucial role in preventing nerve compression. Workstations should be set up to promote neutral postures and minimize repetitive strain. Chairs should provide adequate lumbar support and allow feet to rest flat on the floor.
Computer monitors should be positioned at eye level to reduce neck strain. Keyboards and mice should be placed to keep wrists in a neutral position. Regular breaks are essential to avoid prolonged static postures.
For jobs requiring repetitive motions, task rotation can help distribute stress across different muscle groups. Using ergonomic tools designed to reduce hand and wrist strain can also be beneficial.
Exercise and Strengthening
Regular physical activity helps maintain muscle strength and flexibility, reducing the risk of nerve compression. Stretching exercises targeting areas prone to compression, such as the wrists, elbows, and shoulders, can improve flexibility and circulation.
Strength training exercises focusing on the core and upper body can improve posture and support proper alignment. Yoga and Pilates can enhance overall body awareness and promote balanced muscle development.
Cardiovascular exercise improves circulation, which is vital for nerve health. Activities like swimming or cycling provide low-impact options that are gentle on joints while promoting overall fitness.
Incorporating specific exercises to strengthen muscles around vulnerable areas, such as wrist curls for carpal tunnel prevention, can provide targeted protection against nerve compression.
Frequently Asked Questions
What are the common symptoms indicative of nerve compression?
Typical symptoms include numbness, tingling, and pain in the affected area. Muscle weakness may occur in some cases. Patients often report a burning or “pins and needles” sensation along the path of the compressed nerve.
What treatment options are available for nerve compression syndrome?
Conservative treatments include rest, physical therapy, and anti-inflammatory medications. In more severe cases, corticosteroid injections may be recommended. Surgery becomes an option when non-invasive methods fail to provide relief.
How long is the recovery period following nerve compression surgery?
Recovery time varies depending on the specific procedure and individual factors. Most patients can return to light activities within 2-4 weeks. Full recovery may take several months, with ongoing physical therapy to regain strength and function.
What are the success rates associated with nerve decompression surgery?
Success rates for nerve decompression surgery are generally high. Many patients experience significant improvement in symptoms. Studies show success rates ranging from 70-90%, depending on the specific condition and surgical technique used.
How is a nerve compression diagnosis typically confirmed?
Diagnosis often involves a combination of physical examination and imaging studies. MRI or CT scans can reveal the extent of nerve compression. Electromyography (EMG) and nerve conduction studies may be used to assess nerve function and pinpoint the location of compression.
Can nerve compression syndrome be treated without surgery?
Many cases of nerve compression can be managed without surgery. Conservative treatments like physical therapy, lifestyle modifications, and pain management techniques are often effective. Surgery is typically considered only after non-surgical options have been exhausted.
