Neuroma Surgery
- Miami -
Overview
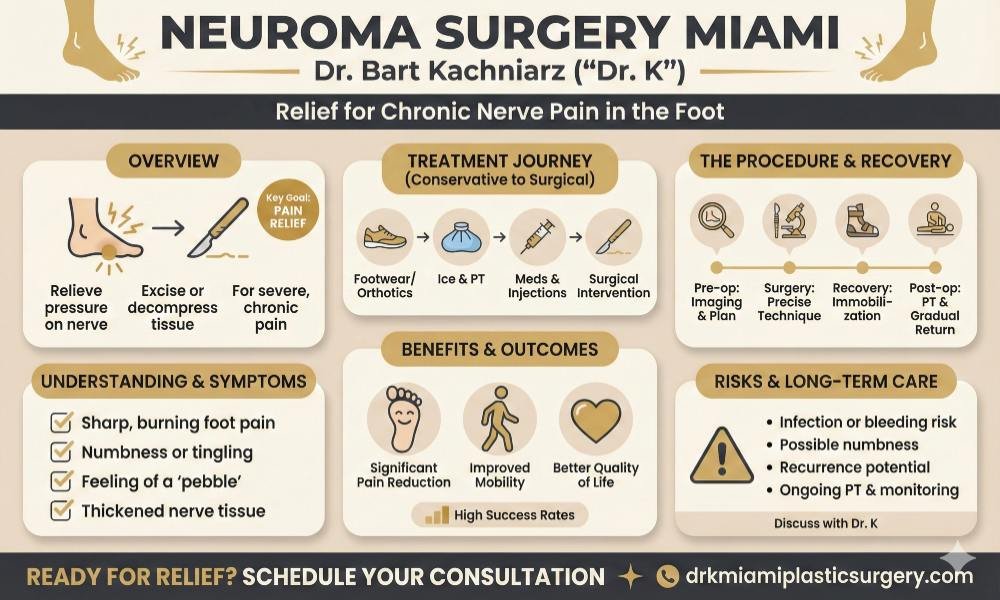
Neuroma pain can be a debilitating condition affecting the feet, often causing sharp, burning sensations in the ball of the foot and toes. While conservative treatments are typically tried first, surgery may become necessary for some patients who do not find relief through other methods.
Surgical intervention for neuroma pain aims to relieve pressure on the affected nerve, either by removing the thickened tissue or decompressing surrounding structures. The most common procedure for Morton’s neuroma involves excising the enlarged nerve tissue. However, decompression surgery, which cuts nearby ligaments to reduce pressure, is sometimes performed as an alternative approach.
It’s important to note that neuroma surgery is not without risks. Some patients may experience persistent post-surgical pain or complications.
Get in touch with us at Dr K Miami Plastic Surgery for your consultation today and see if surgery is the right option for you.


Understanding Neuroma Pain
A neuroma is a thickening of nerve tissue that can develop in various parts of the body. The most common type is Morton’s neuroma, which occurs between the third and fourth toes. Other types include acoustic neuromas in the inner ear and traumatic neuromas resulting from injury.
Neuromas form when nerves are subjected to pressure or irritation, leading to swelling and thickening. This enlarged nerve tissue can cause pain, numbness, and tingling sensations in the affected area.
Symptoms and Diagnosis
Common symptoms of neuroma pain include:
- Sharp, burning pain in the affected area
- Numbness or tingling sensations
- Feeling of a small pebble under the foot (for Morton’s neuroma)
- Pain that worsens with activity or when wearing tight shoes
Diagnosis typically involves a physical examination and patient history. Doctors may apply pressure to the affected area to reproduce symptoms. Imaging tests like MRI or ultrasound can help confirm the diagnosis and rule out other conditions.
Risk Factors and Causes
Several factors can increase the risk of developing neuromas:
- Foot deformities (e.g., high arches, flat feet)
- Wearing ill-fitting or high-heeled shoes
- Repetitive trauma or pressure on the affected area
- Certain sports activities (e.g., running, court sports)
Causes often involve repeated nerve irritation or compression. In Morton’s neuroma, the nerve between the toes becomes compressed when walking. Occupations requiring prolonged standing or repetitive motions can also contribute to neuroma formation.
Genetics may play a role in some cases, particularly with acoustic neuromas. Understanding these risk factors can help individuals take preventive measures and seek early treatment when symptoms arise.
Treatment Options
Non-surgical options are typically the first line of treatment for neuroma pain. These include:
- Footwear modifications: Wearing wide, low-heeled shoes with a spacious toe box
- Orthotic devices: Custom or over-the-counter inserts to redistribute pressure
- Activity modification: Avoiding activities that exacerbate symptoms
- Ice therapy: Applying cold packs to reduce inflammation
Patients often find relief through a combination of these conservative measures. Physical therapy exercises may also help strengthen foot muscles and improve flexibility.
Pain Management
When conservative treatments prove insufficient, pain management techniques can provide relief:
- Oral medications: NSAIDs or prescription analgesics to reduce pain and inflammation
- Corticosteroid injections: Local injections to decrease swelling and alleviate pain
- Nerve blocks: Temporary numbing of the affected nerve to interrupt pain signals
These interventions aim to control symptoms and improve function. Doctors may recommend a series of injections or a combination of medication types for optimal results.
Alternative Therapies
Some patients explore alternative therapies to complement traditional treatments:
- Acupuncture: Fine needles inserted at specific points to reduce pain
- Massage therapy: Targeted manipulation to improve circulation and reduce tension
- Ultrasound therapy: Sound waves applied to the affected area to promote healing
While scientific evidence supporting these methods varies, some individuals report significant symptom improvement. It’s essential to consult with a healthcare provider before pursuing alternative treatments to ensure safety and appropriateness.


Meet Your Doctor
With years of experience in the field of plastic surgery, Dr. K has built a reputation as one of Miami’s premier plastic surgeons.
His journey into medicine began with a passion for helping others and a keen eye for detail—qualities that have defined his career ever since, but what truly sets him apart is his genuine care for each patient who walks through our doors.
SEE WHAT WE CAN DO FOR YOU
Surgical Interventions
Surgical intervention becomes necessary when non-operative treatments fail to provide adequate pain relief. Patients with severe, chronic pain that significantly impacts daily activities are prime candidates. Diagnostic nerve blocks can help confirm the neuroma’s location and determine if surgery might be beneficial.
Imaging studies, such as ultrasound or MRI, may be used to visualize the neuroma and assess its size and location. The decision to pursue surgery also depends on the patient’s overall health, expectations, and willingness to undergo the procedure and recovery process.

Preoperative Considerations
A thorough preoperative evaluation is crucial for optimal surgical outcomes. This includes a detailed medical history, physical examination, and assessment of the patient’s pain levels and functional limitations.
Key considerations:
- Patient’s overall health status
- Medications, including blood thinners
- Previous treatments and their effectiveness
- Realistic expectations for pain relief and recovery
Preoperative imaging helps surgeons plan the procedure and identify any anatomical variations. Patient education about the surgery, potential risks, and expected recovery timeline is essential for informed decision-making.
Types of Surgical Procedures
Several surgical approaches are available for neuroma treatment:
- Neuroma excision: Removal of the damaged nerve segment
- Nerve transposition: Relocating the nerve to a less irritated area
- Nerve repair: Reconnecting severed nerve ends
- Neurolysis: Freeing the nerve from surrounding scar tissue
The choice of procedure depends on the neuroma’s location, size, and specific patient factors. In some cases, a combination of techniques may be employed for optimal results.
Intraoperative Techniques
Precise surgical techniques are crucial for successful neuroma treatment. Surgeons use magnification devices to visualize the affected nerve and surrounding structures. Careful dissection helps minimize damage to healthy tissue.
Key intraoperative steps:
- Identification and isolation of the affected nerve
- Removal of the neuroma, if applicable
- Nerve reconstruction or relocation, as needed
- Use of specialized nerve wraps or caps to prevent neuroma recurrence
Some surgeons employ intraoperative nerve stimulation to confirm proper nerve function. Meticulous hemostasis and closure techniques help reduce the risk of postoperative complications.
Postoperative Care
Proper postoperative care is essential for optimal healing and pain relief. Patients typically require a period of immobilization and protected weight-bearing, depending on the surgical site. Pain management strategies may include medications, ice therapy, and elevation.
Key postoperative considerations:
- Wound care and dressing changes
- Gradual return to activities as directed by the surgeon
- Physical therapy to improve strength and range of motion
- Follow-up appointments to monitor healing and address any concerns
Patients should be aware that complete pain relief may take several months. Ongoing communication with the surgical team is crucial for addressing any postoperative issues and ensuring the best possible outcome.
Outcomes and Prognosis
Surgical interventions for painful neuromas show promising results for many patients. Studies indicate that a significant percentage of individuals experience pain reduction following neuroma resection and reconstruction procedures. One research found improvements in pain-related symptoms for all patients after surgery, with a decrease in pain medication use from 65% to 23%.
Pain relief is often the primary goal of neuroma surgery. While complete elimination of pain is not always achievable, many patients report substantial improvements in their quality of life post-surgery.
Factors influencing success rates include:
- Surgical technique employed
- Surgeon’s expertise
- Patient’s overall health
- Duration of symptoms prior to surgery

Potential Complications
As with any surgical procedure, neuroma pain surgery carries certain risks. Potential complications may include:
- Infection at the surgical site
- Bleeding or hematoma formation
- Nerve damage leading to sensory disturbances
- Development of a new neuroma at the surgical site
- Persistent or recurrent pain
In some cases, patients may experience temporary loss of sensation in the affected area. This usually improves over time as the nerve heals and regenerates.
It’s important to note that while complications are possible, they are relatively uncommon when the surgery is performed by experienced specialists.
Long-Term Management
Long-term management following neuroma pain surgery is crucial for optimal outcomes. Patients often require ongoing care and follow-up appointments to monitor progress and address any residual issues.
Key aspects of long-term management include:
- Physical therapy to improve function and reduce stiffness
- Pain management techniques, such as medication or nerve blocks
- Regular check-ups to assess healing and identify potential complications
Some patients may benefit from additional interventions or therapies if symptoms persist. These might include:
- Revision surgery in case of recurrence
- Alternative pain management strategies
- Psychological support to cope with chronic pain
Patient education plays a vital role in long-term management. Understanding proper wound care, activity restrictions, and warning signs of complications empowers patients to actively participate in their recovery process.
Advancements in Treatment
Advanced imaging techniques now allow surgeons to precisely locate neuromas, improving surgical accuracy. Ultrasound-guided procedures enable minimally invasive interventions with smaller incisions and faster recovery times.
Nerve capping has emerged as a promising technique. This involves covering the nerve end with a protective barrier to prevent neuroma reformation. Materials like processed nerve allografts facilitate axonal growth and nerve regeneration without donor site morbidity.
Targeted muscle reinnervation (TMR) is gaining traction for treating neuromas in amputees. This procedure redirects cut nerve endings to nearby muscles, reducing phantom limb pain and improving prosthetic control.
Patient Education and Support
Effective patient education is crucial for individuals facing neuroma pain surgery. Healthcare providers should offer clear, detailed information about the procedure, potential outcomes, and recovery process.
Pre-operative counseling helps patients set realistic expectations. This includes discussing pain management strategies, potential complications, and the importance of follow-up care.
Written materials and visual aids can reinforce verbal explanations. These may include:
- Diagrams of nerve anatomy
- Step-by-step surgical procedure descriptions
- Post-operative care instructions
Support groups can be valuable resources for patients. Connecting with others who have undergone similar procedures can provide emotional support and practical advice.
Physical therapy plays a key role in recovery. Patients should understand the importance of adhering to prescribed exercises and attending follow-up appointments.
Pain management education is essential. Patients need to learn about:
- Proper use of prescribed medications
- Non-pharmacological pain relief techniques
- Signs that indicate the need for medical attention
Occupational therapy may be necessary to help patients adapt to any functional changes. This can include training in daily living activities and workplace modifications.

Clinical Guidelines and Best Practices
Surgical management of neuroma pain requires a carefully considered approach. The American Association of Neuromuscular & Electrodiagnostic Medicine recommends a thorough evaluation before pursuing surgical intervention.
Diagnostic imaging, including ultrasound and MRI, is essential for accurate neuroma identification. These tests help determine the size and location of the neuroma, guiding surgical planning.
Conservative treatments should be attempted before surgery. These may include:
- Orthotics and footwear modifications
- Physical therapy
- Corticosteroid injections
- Radiofrequency ablation
When surgery is deemed necessary, excision of the neuroma is a common approach. However, newer techniques focus on nerve preservation and reconstruction.
The surgical algorithm for neuroma management has evolved. Current best practices emphasize:
- Precise nerve identification
- Minimal tissue disruption
- Nerve end protection or redirection
Post-operative pain management is crucial. A multimodal approach combining local anesthetics, nerve blocks, and systemic medications is recommended.
Follow-up care should include regular assessments of pain levels and functional outcomes. Physical therapy may be prescribed to aid in recovery and prevent recurrence.
Surgeons should stay updated on emerging techniques and research findings to provide optimal care for patients with neuroma pain.
Multidisciplinary Approach to Care
Treating neuroma pain effectively often requires a team of specialists working together. This collaborative approach ensures patients receive comprehensive care addressing all aspects of their condition.
A typical multidisciplinary team for neuroma pain may include:
- Neurologists
- Pain management specialists
- Surgeons
- Physical therapists
- Psychological therapists
Each expert brings unique skills and perspectives to develop an optimal treatment plan. Neurologists assess nerve function and damage. Pain specialists manage symptoms using various techniques.
Surgeons evaluate the need for operative intervention and perform procedures when necessary. Physical therapists help improve mobility and function. Psychological therapists address the emotional impact of chronic pain.
This integrated approach allows for more accurate diagnosis and tailored treatment strategies. It can help prevent unnecessary surgeries and improve outcomes for patients with neuroma pain.
Coordination between team members is crucial. Regular communication ensures all aspects of a patient’s care are aligned. This holistic strategy often leads to better pain relief and improved quality of life.
Patients benefit from having multiple expert opinions and treatment options. The team can adjust the care plan as needed based on the individual’s response and progress.
