Excess skin and fat hanging from your lower abdomen creates more than cosmetic concerns. This condition—medically termed pannus stomach—leads to recurring skin infections, chronic back pain, and mobility restrictions that significantly impact daily life.
The reality: diet and exercise reduce fat effectively, but permanently overstretched skin requires medical intervention. Board-certified plastic surgeon Dr. Bart Kachniarz specializes in surgical treatment for apron belly at Dr. K Miami. With advanced training from Harvard Medical School and Johns Hopkins Hospital, Dr. Kachniarz performs panniculectomy and abdominoplasty procedures using techniques refined at leading academic medical centers.
This guide examines proven solutions—from targeted nutrition and proper skin care to surgical options—helping you make informed decisions about your treatment path.
What Is an Apron Belly?
Apron belly refers to excess fat and skin tissue hanging from the abdomen, extending over the lower abdomen and potentially reaching the pubic area in moderate cases or down to the thighs in severe instances. Medical professionals diagnose this condition when overhanging tissue reaches the pubic hairline.
The tissue consists of subcutaneous fat and overstretched skin that has lost elasticity. Unlike regular abdominal fat that remains firm, apron belly involves fat that hangs and moves separately from the core. Severe cases interfere with mobility and daily activities while creating friction between skin folds that leads to discomfort and health complications.
Medical Classification: Pannus Grades
Healthcare providers classify apron belly into five grades based on tissue extension:
Grade 1: Pannus extends to cover the pubic hairline
Grade 2: Tissue hangs to cover the genitals
Grade 3: Pannus reaches the upper thigh
Grade 4: Tissue extends to the mid-thigh
Grade 5: Pannus hangs to the knee or below
Severity determines treatment approaches and potential complications. Grade 1 or 2 may respond to noninvasive treatments, while Grade 3 or higher typically requires surgical intervention. Insurance companies use this terminology when evaluating whether surgical removal qualifies as medically necessary rather than cosmetic, with coverage depending on documented chronic infections, skin breakdown, or mobility limitations.
What Can Cause an Apron Belly?
Understanding the causes of apron belly helps identify appropriate treatment strategies.
1. Pregnancy and Postpartum Changes
Abdominal muscles and skin stretch significantly during pregnancy to accommodate a growing baby. This expansion can lead to diastasis recti—a condition where abdominal muscles separate along the midline—weakening connective tissue and reducing skin elasticity.
After delivery, the uterus requires approximately six weeks to return to pre-pregnancy dimensions, while the abdominal area may need several months to over a year for noticeable improvement. Women who gain excessive weight during pregnancy face higher risks of developing postpartum apron belly. Multiple pregnancies increase likelihood through repeated stretching that compromises skin elasticity and abdominal muscle integrity.
Previous cesarean sections contribute to apron belly development through scar tissue formation. C-section shelf results specifically from scar tissue along the incision line, creating a distinct break where tissue accumulates and folds over the surgical site.
2. Weight Gain and Obesity
Obesity causes fat accumulation both under the skin and around internal organs. Carrying excess weight in the abdominal area places constant downward pressure on tissues, contributing to the characteristic hanging appearance.
Visceral fat surrounds internal organs and pushes the abdominal wall outward, while subcutaneous fat creates the visible overhang.
3. Significant Weight Loss and Bariatric Surgery
Rapid or substantial weight loss—particularly after bariatric surgery—often leaves behind excess skin. When someone loses 100 pounds or more, skin cannot contract quickly enough to match new body composition. Bariatric surgery patients frequently experience this issue because they lose large amounts of weight in relatively short timeframes.
4. Genetics, Aging, and Hormonal Changes
Genetic factors determine where the body stores fat and how well skin maintains elasticity. Family history often indicates susceptibility to this condition.
Aging naturally reduces collagen and elastin production in skin, making it thinner and less able to retract after stretching. Hormonal changes during menopause shift fat distribution toward the abdomen in women. Some refer to this as “meno belly” when it develops during menopausal transition.
Certain medical conditions increase apron belly risk by affecting weight regulation and fat distribution. Hypothyroidism, polycystic ovary syndrome (PCOS), Cushing’s syndrome, and diabetes make maintaining healthy weight particularly challenging. Individuals with these conditions should work closely with healthcare providers to manage both the underlying disorder and associated body composition changes.
5. Weight Fluctuations and Yo-Yo Dieting
Repeated cycles of weight gain and loss place individuals at heightened risk for developing apron belly. Each stretching episode gradually weakens skin’s structural integrity, reducing its ability to contract after subsequent weight changes. This cumulative damage means each weight loss becomes progressively more likely to result in permanent skin laxity.
Health Risks
Apron belly creates physical health problems ranging from skin infections to chronic disease risks while affecting mental wellbeing.
Skin Infections and Irritation
Overlapping skin folds create an environment prone to moisture buildup and friction. Trapped moisture becomes a breeding ground for bacterial and fungal infections. The warm, enclosed environment promotes proliferation, frequently resulting in persistent rashes characterized by redness, discomfort, and odor.
Cellulitis represents one serious bacterial infection affecting deeper skin layers that can spread rapidly if untreated. Individuals may notice redness, warmth, swelling, and pain. Intertrigo is another common condition occurring when skin rubs against skin in folds, appearing as red, raw-looking patches with itching and burning sensations.
Additional complications include:
- Skin sores and ulcers from persistent irritation
- Heat rash from reduced air circulation
- Chafing that leads to broken skin
- Persistent odor from bacterial overgrowth
Back Pain and Mobility Issues
The weight of excess abdominal tissue pulling forward places considerable strain on the spine and surrounding muscles. Body biomechanics shift to compensate for anterior weight, forcing lower back muscles to work harder maintaining balance. Over time, constant strain leads to chronic pain and muscle fatigue.
Additional anterior weight shifts the body’s center of gravity forward, creating biomechanical stress on hip joints alongside spinal strain. Simple activities like standing for extended periods, walking, or bending become challenging. Severe cases affect ability to rise from chairs or find comfortable lying positions.
Forward weight distribution can increase intra-abdominal pressure, potentially leading to ventral hernias—when abdominal tissue or intestinal segments protrude through weakened spots in the abdominal wall, requiring medical evaluation and possible surgical repair. Restricted movement often leads to reduced physical activity levels. When regular exercise becomes uncomfortable, individuals may adopt increasingly sedentary lifestyles, creating a cycle where decreased activity makes weight management harder.
Metabolic and Chronic Health Risks
When obesity causes apron belly, excess visceral fat increases risk for serious metabolic conditions. Type 2 diabetes risk rises significantly with increased abdominal fat, as this tissue affects insulin sensitivity and blood sugar regulation. Research links excessive abdominal fat—particularly visceral deposits—with elevated ovarian cancer risk.
A BMI of 40 or more, which often accompanies severe apron belly (pannus morbidus), substantially elevates these risks. Additional concerns include:
- Hypertension
- High cholesterol and triglycerides
- Stroke risk
- Sleep apnea
- Fatty liver disease
- Heart disease
Fat tissue in the abdominal area produces inflammatory compounds that actively contribute to disease progression rather than simply serving as passive storage.
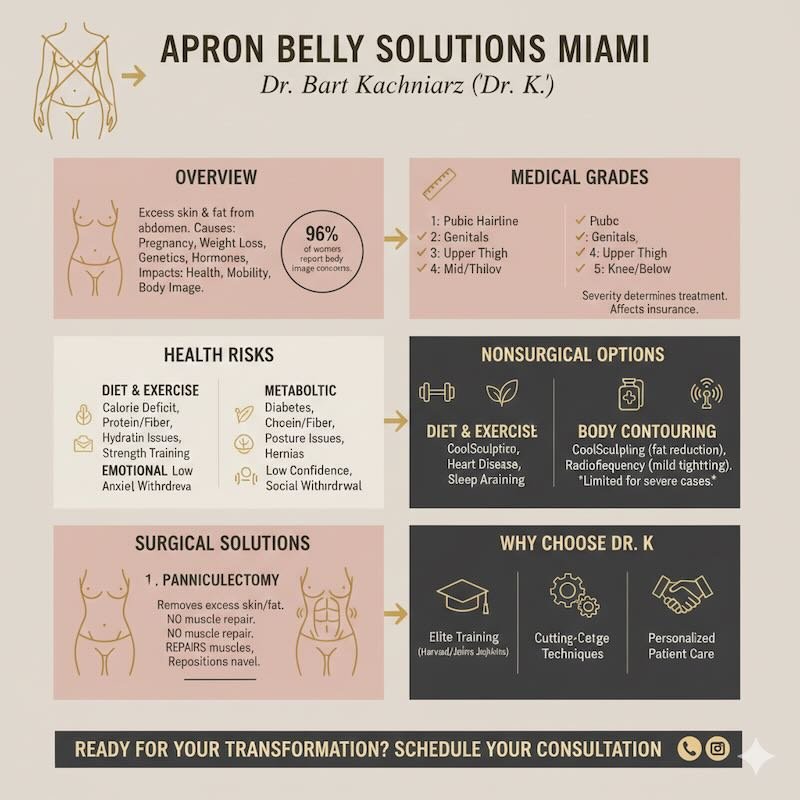
Nonsurgical Strategies to Get Rid of Apron Belly
Reducing apron belly without surgery requires combining strategic weight loss, nutritional improvements, and lifestyle modifications focused on sustainable habits.
Creating an Effective Calorie Deficit
Weight loss through calorie deficit forms the foundation for reducing apron belly fat. A calorie deficit occurs when the body burns more calories than it consumes, forcing it to use stored fat for energy.
Creating a deficit of 500–750 calories per day typically results in losing 1–2 pounds per week—a rate considered safe and sustainable. The body cannot target fat loss in specific areas, so overall weight reduction is necessary to see improvement in the abdominal region.
Key factors for success:
- Calculate daily caloric needs based on age, weight, height, and activity level
- Reduce intake by 500–750 calories from maintenance level
- Monitor progress weekly through measurements and photos
- Adjust calories as weight decreases to maintain steady loss
- Track daily calorie intake using a food diary or app to increase awareness of eating patterns
Nutrition and Diet Optimization
A healthy diet focused on whole, nutrient-dense foods supports weight loss while providing essential vitamins and minerals. Nutrition quality matters as much as calorie quantity.
- Protein: Include lean protein at every meal—chicken breast, turkey, fish, eggs, Greek yogurt, and legumes. Protein helps preserve muscle mass during weight loss and increases satiety. Most adults need 0.7–1 gram of protein per pound of body weight when losing fat.
- Fiber: Consume 25–30 grams daily from vegetables, fruits, and whole grains. Foods like oats, quinoa, brown rice, berries, and leafy greens provide sustained energy without blood sugar spikes, improving digestion and controlling hunger.
- Processed foods: Reduce items containing excess sodium, added sugars, and unhealthy fats that contribute to inflammation and fat storage. Replace packaged snacks with whole food alternatives.
- Home cooking: Home-cooked meals contain fewer calories and less added sugar compared to restaurant meals or prepared frozen options, making this practice particularly valuable for reducing abdominal fat.
Hydration and Anti-Inflammatory Strategies
Water helps the body process and eliminate fat byproducts while supporting cellular functions. Drinking 15.5 cups (3.7 liters) of total fluids for men and 11.5 cups (2.7 liters) for women daily, which includes water from food, is a baseline recommendation, with individual needs varying based on activity level, climate, and body size. People often mistake thirst for hunger, leading to unnecessary calorie consumption.
- Drinking 16 ounces of water 30 minutes before eating helps with portion control.
- Anti-inflammatory foods: Include fatty fish rich in omega-3s, berries, leafy greens, nuts, and olive oil. Chronic inflammation interferes with weight loss and contributes to fat storage around the abdomen.
- Alcohol limitation: Alcohol provides 7 calories per gram with no nutritional value and can impair fat metabolism for up to 24 hours after consumption.
- Additional fluids: Green tea and herbal teas count toward daily fluid intake while providing antioxidants that may support fat loss. Avoid sugary beverages—liquid calories don’t provide satiety and can add hundreds of unnecessary calories daily.
Compression Garments and Support
Compression garments worn regularly during weight loss may support skin adaptation as body composition changes. Support bands that lift hanging tissue higher on the body may ease walking and reduce back discomfort. However, these bands can trap heat and moisture against skin, potentially increasing irritation risk.
Supportive undergarments provide gentle, consistent pressure that can help reduce friction-related discomfort while potentially assisting skin retraction. Choose breathable materials and ensure proper fit to avoid creating additional skin irritation in fold areas. Proper hygiene becomes even more critical when using support garments.
Compression support works best as a temporary measure during early recovery rather than a permanent solution. These garments should fit snugly without excessive tightness and require consultation with your healthcare provider before use, particularly following cesarean delivery. The goal remains building sufficient core strength to eventually eliminate dependence on external support.
Exercise Strategies for Apron Belly
No exercise can directly target fat loss in the abdominal area alone—fat reduction occurs throughout the body as overall body weight decreases. The abdomen contains two distinct fat layers compared to single layers in arms and legs, making this area particularly resistant to isolated approaches. Your body draws energy from stored fat throughout the entire body during physical activity, not just from the specific area being exercised.
Strength training exercises that build lean muscle mass are particularly beneficial. Squats, push-ups, rows, and presses help increase metabolism since muscle tissue is more metabolically active than fat tissue, burning approximately 6 calories per pound daily compared to 2–3 calories for fat. While the difference is modest at rest, having more muscle mass increases overall daily calorie expenditure through improved activity capacity and enhanced insulin sensitivity. Perform these exercises 2–3 times per week for optimal results.
Full-body compound movements like squats, deadlifts, overhead presses, and pull-ups engage core muscles significantly when performed with correct form. Building your strength routine around these exercises, then supplementing with occasional targeted abdominal work, creates more effective fat reduction than isolated core exercises alone.
Why Diet and Exercise Alone May Not Remove Your Apron Belly
While lifestyle modifications effectively reduce abdominal fat, they cannot restore elasticity to permanently overstretched skin. Once skin has been stretched beyond its capacity for extended periods, structural damage to elastic fibers becomes irreversible. This explains why some individuals see fat reduction but persistent skin overhang despite dedicated effort.
Additionally, stubborn fat in the abdominal area can prove particularly resistant to diet and exercise, especially when hormonal factors contribute to its accumulation. Metabolism naturally slows with age, further reducing the rate at which the body burns stored fat. Aging also reduces muscle mass and alters immune function.
Despite these physiological changes, targeted nutrition strategies and appropriate exercise protocols remain effective for those committed to reducing abdominal fat.
Noninvasive Body Contouring Procedures for Addressing Apron Belly
Noninvasive treatments work best for patients with good skin elasticity and minimal loose skin. These procedures target fat reduction rather than skin removal.
Cryolipolysis (CoolSculpting)
Cryolipolysis uses controlled cooling to freeze and eliminate fat cells beneath the skin. The body naturally processes these dead cells over 2–3 months. Results typically show a 20–25% reduction in the treated fat layer.
However, cryolipolysis cannot address sagging skin or significant tissue overhang.
Radiofrequency Treatments
Radiofrequency treatments deliver heat energy to deeper skin layers, stimulating collagen production and promoting mild skin tightening. Multiple sessions are usually required, with results appearing gradually over several months. The skin tightening effect remains limited compared to surgical options.
These technologies are not suitable for individuals who are nursing or those with obesity, and may address multiple body areas simultaneously beyond just the abdomen.
Fat freezing and similar technologies may reduce some fat deposits but cannot remove the substantial excess skin characteristic of moderate to severe apron belly. Patients with Grade 1 apron belly may see modest improvements, while those with Grade 2 or higher typically require surgical intervention for meaningful results.
Surgical Options to Remove Apron Belly
Board-certified plastic surgeon Dr. Bart Kachniarz performs both panniculectomy and abdominoplasty procedures at Dr. K Miami using advanced techniques developed through training at Harvard Medical School and Johns Hopkins Hospital.
Panniculectomy: Targeted Tissue Removal
Panniculectomy focuses exclusively on removing the hanging panniculus of skin and fat. The surgeon makes a horizontal incision from hip to hip, removes excess skin and fat from the overhanging tissue (often 10–30+ pounds), and closes the remaining area. This procedure does not tighten abdominal muscles or reposition the belly button—it simply removes the problematic apron itself.
Panniculectomy targets exclusively the lower abdominal hanging tissue without addressing the upper or middle abdomen. Following surgery, patients typically wear an elastic support garment or abdominal binder for several weeks to provide support during healing, minimize swelling, and help remaining tissue conform to its new contour.
Abdominoplasty For Comprehensive Rejuvenation
Abdominoplasty provides comprehensive abdominal rejuvenation beyond simple tissue removal. The procedure removes excess skin, repairs separated abdominal muscles, repositions the belly button, and contours the entire midsection. A mini tummy tuck addresses loose skin below the navel through a shorter incision with faster recovery of 2–3 weeks.
Advanced techniques combining abdominoplasty with liposuction can sculpt surrounding areas for seamless results. When apron belly consists primarily of hanging tissue rather than localized fat deposits, liposuction alone rarely provides satisfactory results and typically requires combination with skin removal procedures.
Some patients benefit from combining panniculectomy with abdominoplasty elements, creating customized surgical plans that address both hanging tissue and comprehensive muscle tightening or contouring needs. Your surgeon evaluates whether this combined approach better serves your specific anatomy and goals.
Get Expert Care for Your Apron Belly in Miami
If you’re struggling with apron belly and considering surgical treatment, Dr. K Miami offers personalized consultations to discuss your options. With dual training from Harvard Medical School and Johns Hopkins Hospital, Dr. Bart Kachniarz brings award-winning expertise to every procedure.
Schedule your free consultation today to explore whether panniculectomy or abdominoplasty is right for you.



